Pathologic Evaluation of a Surgical Resection Specimen
We have already covered the basic pathology report in the first update. This section details each of the criteria for large resections. You may see some complicated terms in your pathology report. For example: what does the “AJCC 8th edition” or “FIGO” stage mean? Why do we include ‘lymphovascular invasion’ or ‘perineural invasion’? The goal of the “For your patients section” on this website is to effectively translate some complicated pathology terminology. This month, we review the pathologic evaluation of a breast resection specimen.
Breast Cancer
Breast cancer is the most common cancer among women in Trinidad and Tobago. You may have been diagnosed with it on a biopsy and then proceeded to a resection (wide local excision, simple mastectomy, modified radical mastectomy and radical mastectomy all come under the resection umbrella)
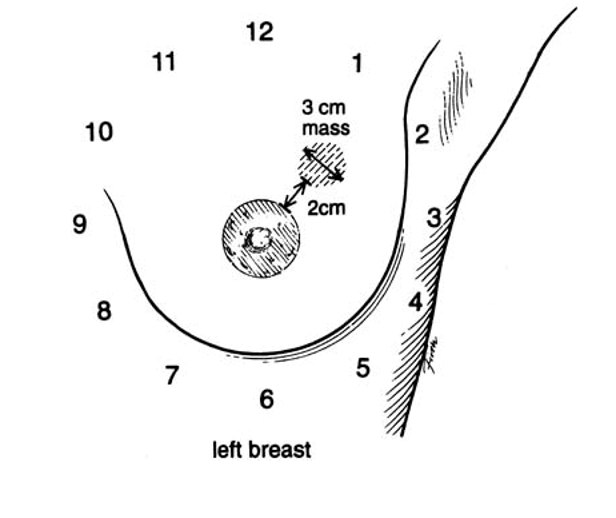
In the illustration on the right, there’s a tumour at 1 o’clock in the left breast. It’s also in the “upper outer quadrant” if you were to divide the breast into four quarters. After your surgery, your pathologist will review that specimen for the criteria discussed on the following pages.
What happens to the specimen in the lab
- Before the microscopic evaluation we do a gross description of the specimen to document:
- Size of the tumor
- Where the tumour is and if it’s invading into the skin or posterior skeletal muscle.
- If it’s completely taken out and how far away the tumor is from the cut edges (the “margins”)
- Lymph nodes if we received an ‘axillary node dissection’ (lymph nodes from the armpit).
- We then take sections of the tissue to evaluate the tissue microscopically to document:
- The grade of the tumour – discussed in the subsequent slides
- Whether the tumour is inside blood vessels (“lymphovascular invasion”)
- Whether the tumour was completely taken out (measuring how close it comes to the margins)
- The microscopic distance to the margins is particularly important in breast carcinomas and should be documented in every report as that will inform your surgeon on next steps.
- Two important lines include the grade and the stage (at the bottom some reports will have “AJCC 8th edition” or “pT__ N__ M__). Your surgeon will be able to tell you the stage of the tumour as it involves several components of the pathology report including:
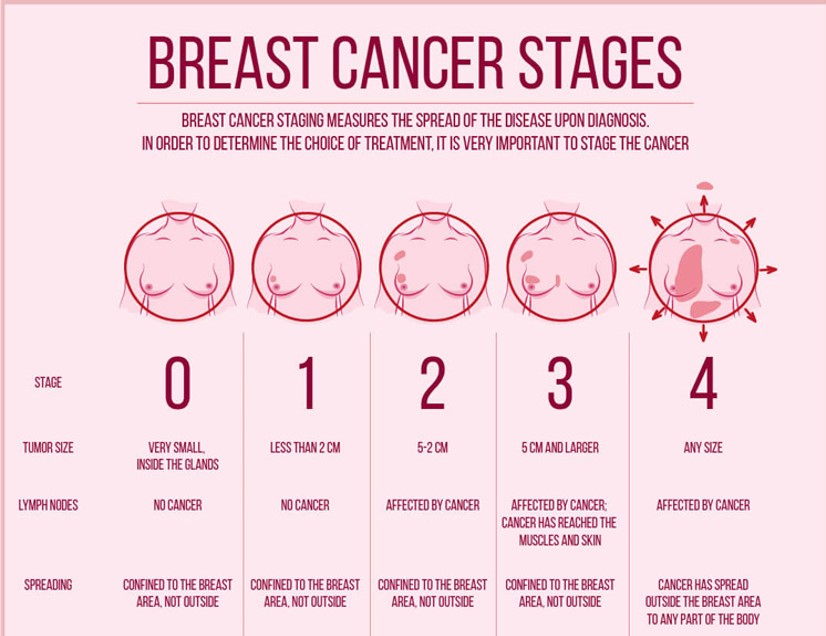
“T” stage – The size of the tumour and if it involves the skin
“N” stage – how many lymph nodes are involved, if any
“M” stage – if any tumour is present outside of the breast
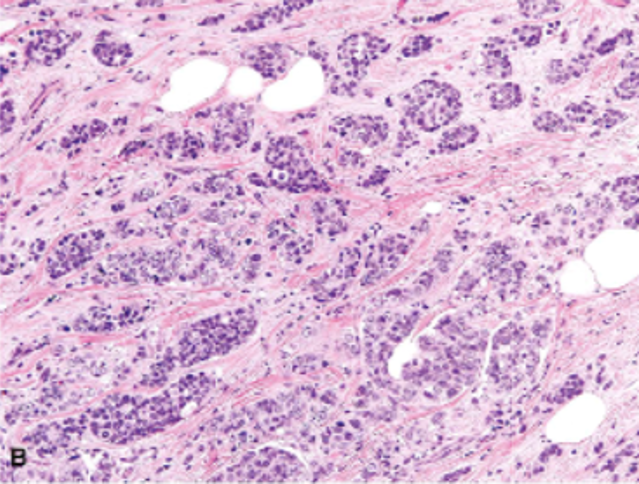
Grading Breast Cancers
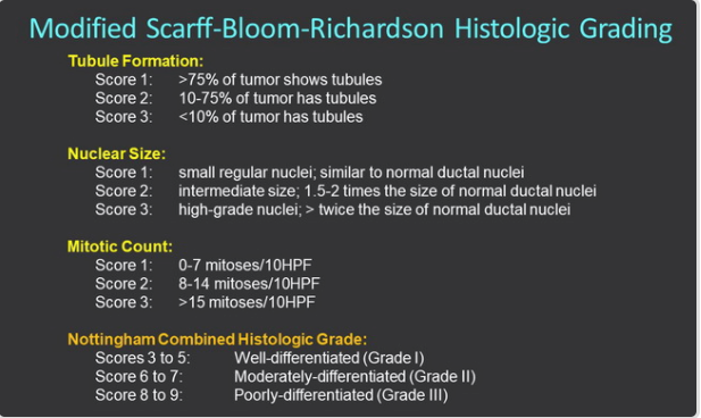
The pathologist looks at and scores several things under the microscope to see how aggressive your tumour is:
Tubules: Well behaved breast cancers look like circles or tubules under the microscope, the more there are of these, the lower the score.
Nuclear size: The core of the cell is a nucleus, well behaved cancers have small nuclei, the larger they are, the higher the score.
Mitotic count: Cancer cells can grow at a rapid rate by splitting into two. The pathologist can see this division and count the number of cells splitting into two – this is called the mitotic count. The higher this count, the higher the score.
The scores of each of these criteria are added up to assess the grade of the tumour. See the formal chart on the right for the Nottingham Combined Histologic Grade.
Here are examples of scoring for tubules
Lots of tubules – 1 point
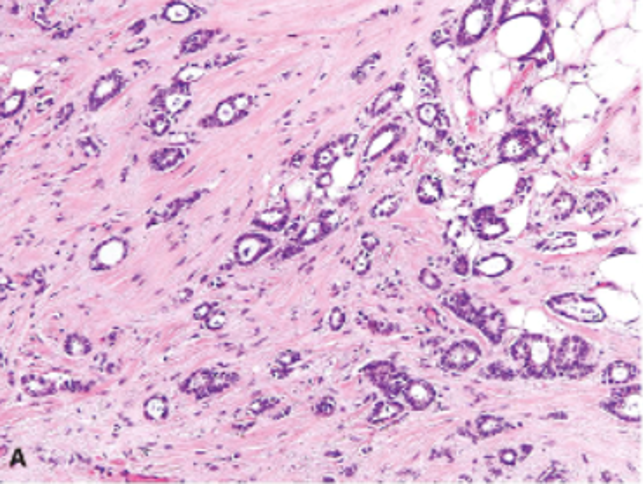
No tubules – 3 points
T stage: We measure the size of the tumour grossly (before taking sections for microscopy) and microscopically. The latter usually fits with the gross measurement. We determine whether the tumour has spread from the ducts of the breast (invasive carcinoma) or confined to the ducts of the breast alone (in situ carcinoma). We also determine whether or not the tumour, if invasive, involves the skin or deep chest muscles.
N stage : We may get lymph nodes associated with the specimen – something called a sentinel node (the first node that the cancer – if it spreads – will go to). We serially section and examine those sentinel nodes to look for any cancer cells within the lymph node. We may also get an entire axillary lymph node dissection – several lymph nodes from the armpit. We examine these lymph nodes for any cancer. If they’re all negative we give it an N0, if one has cancer, we give it an N1a; the more nodes that are positive, the higher that “N” will be.
M stage: Sometimes, your surgeon may notice lesions in the liver, lungs or bone on CT scan and decide to take that out as well. That will contribute to the M stage if the pathologist reviews that specimen. If there is no spread (metastasis) that will be an “M0” but if there are, the “M” stage will be “M1”.
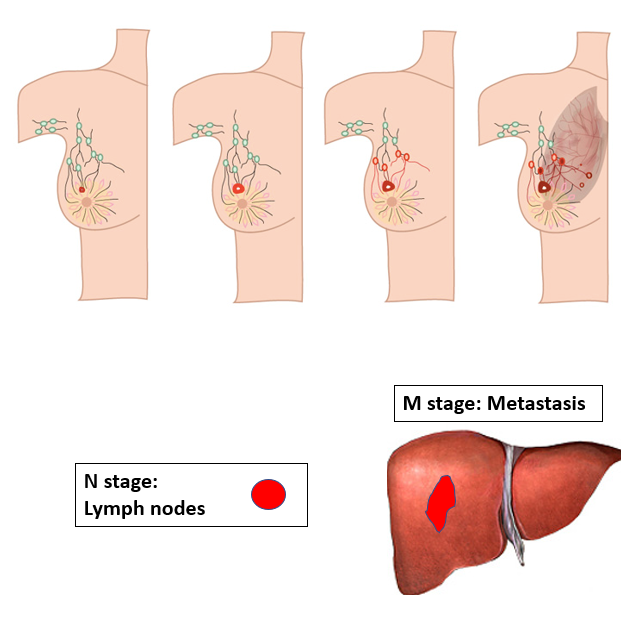
So, is it Stage 1, 2, 3 or 4? With the TNM stage, the surgeon can then say what overall stage the tumour is (see diagram on the right)