We have already covered the basic pathology report in the first update. This section details each of the criteria for large resections. You may see some complicated terms in your pathology report. For example: what does the “AJCC 8th edition” or “FIGO” stage mean? Why do we include ‘lymphovascular invasion’ or ‘perineural invasion’? The goal of the “For your patients section” on this website is to effectively translate some complicated pathology terminology. This will be a series of sorts over the next three months. In this October update we discuss colon cancer and the important things to look for in your pathology report. In November and December we’ll be covering Breast cancer and Endometrial cancer respectively.
Colon Cancer
Colorectal cancers are the third most commonly diagnosed cancers worldwide. You may have been diagnosed with it on a biopsy and then proceeded to a resection (“colectomy”, “hemicolectomy”, ”sigmoidectomy”, “abdominal perineal resection”, “low anterior resection” all come under the resection umbrella)
In the illustration on the right, there’s a tumour in the descending colon. After your surgery, your pathologist will review that specimen for the criteria discussed below.
What happens to the specimen in the lab:
Before the microscopic evaluation we do a gross description of the specimen to document:
- Size of the tumor
- How deep through the wall of the colon it’s invading (we do this microscopically as well)
- If it’s completely taken out and how far away the tumor is from the cut edges (the “margins”)
- The number of lymph nodes we identify in the surrounding tissue
We then take sections of the tissue to evaluate the tissue microscopically to document:
- The grade of the tumour – discussed in the July update
- Whether the tumour is inside blood vessels (“lymphovascular invasion)
- Whether the tumour was completely taken out (measuring how close it comes to the margins).
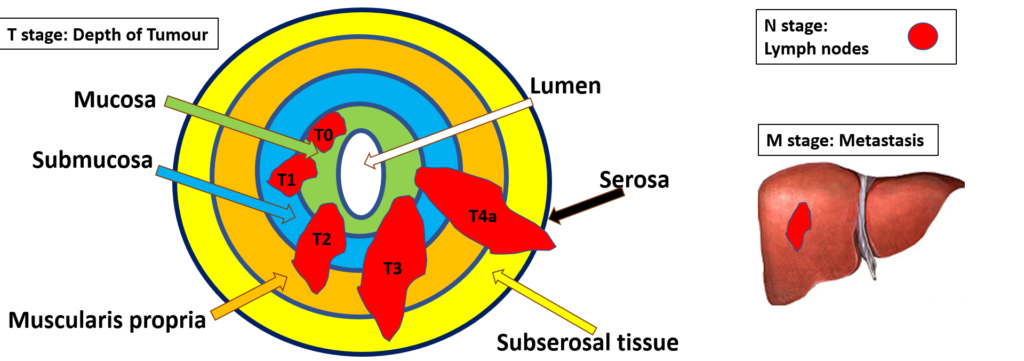
Perhaps the most important line of your report is the line discussing the stage (at the bottom some reports will have “AJCC 8th edition” or “pT__ N__ M__). Your surgeon will be able to tell you the stage of the tumour as it involves several components of the pathology report including:
“T” stage – how deep the tumour invades
“N” stage – how many lymph nodes are involved, if any
“M” stage – if any tumour is present outside of the colon (in the liver for example).
See the illustrations below for a better understanding of what all these stages mean and how they relate to stage 1, 2, 3 and 4 tumours.
T stage: The colon is a tube, and the cancer can be confined to the inner lining of the tube (where it starts) or go through the entire wall of the tube. Involvement of each layer of the wall indicates a higher “T” stage. If the tumour involves the muscularis propria for example it’s a T2, but if it goes all the way through the serosa it’s a T4a
N stage : We aim to sample at least 12 lymph nodes in colon cancer specimens to look for spread of the colon cancer into the surrounding lymph nodes. Lymph nodes are present in the fat that surrounds the colon tube. If there’s no spread that will be an “N0” but, if the cancer has spread to one of the twelve lymph nodes it’s an “N1a”. The more nodes that are positive, the higher the “N” stage.
M stage: Sometimes, your surgeon may notice lesions in the liver on CT scan and decide to take that out as well. That will contribute to the M stage if the pathologist reviews that specimen. If there is no spread (Metastasis) that will be an “M0” but if there are, the “M” stage will be “M1a”, if the tumour involves more than just the liver and the colon, the ”M” stage will be “M1b”.
So, is it Stage 1, 2, 3 or 4?
With the TNM stage, the surgeon can then say what stage the tumour is based on the table below